- Gavi, the Vaccine Alliance, has allocated $1.5 billion, covering only one-third of the estimated $4–5 billion needed.
- Malaria remains a major public health crisis in Africa, accounting for 95% of global malaria deaths, most of which occur among children under five.
- Under current plans, an estimated 2.5 million children will die of malaria unvaccinated by 2030.
ZAMBIA, Lusaka, 28 January 2025 -/African Media Agency(AMA)/- The global health community faces a critical funding shortfall that threatens the timely distribution of malaria vaccines to millions of vulnerable children in Africa, according to a White Paper authored by 1Day Sooner and the Center for Global Development (CGD), informed by conversations with the World Health Organisation (WHO), among other partners. Despite unprecedented progress with malaria vaccines such as R21, a $4 billion funding gap endangers the goal of vaccinating all eligible children by 2030. Gavi, the Vaccine Alliance, has allocated $1.5 billion, covering only one-third of the estimated $4–5 billion needed.
According to the white paper titled “Avoiding Another Lost Decade on Malaria Vaccines,” malaria remains a major public health crisis in Africa, accounting for 95% of global malaria deaths, most of which occur among children under five. Vaccines like R21 offer a transformative, cost-effective solution. Priced at just $3.90 per dose, and with a capacity to save one life for every $4,200 spent, R21 has been lauded as one of the most impactful health interventions in history.
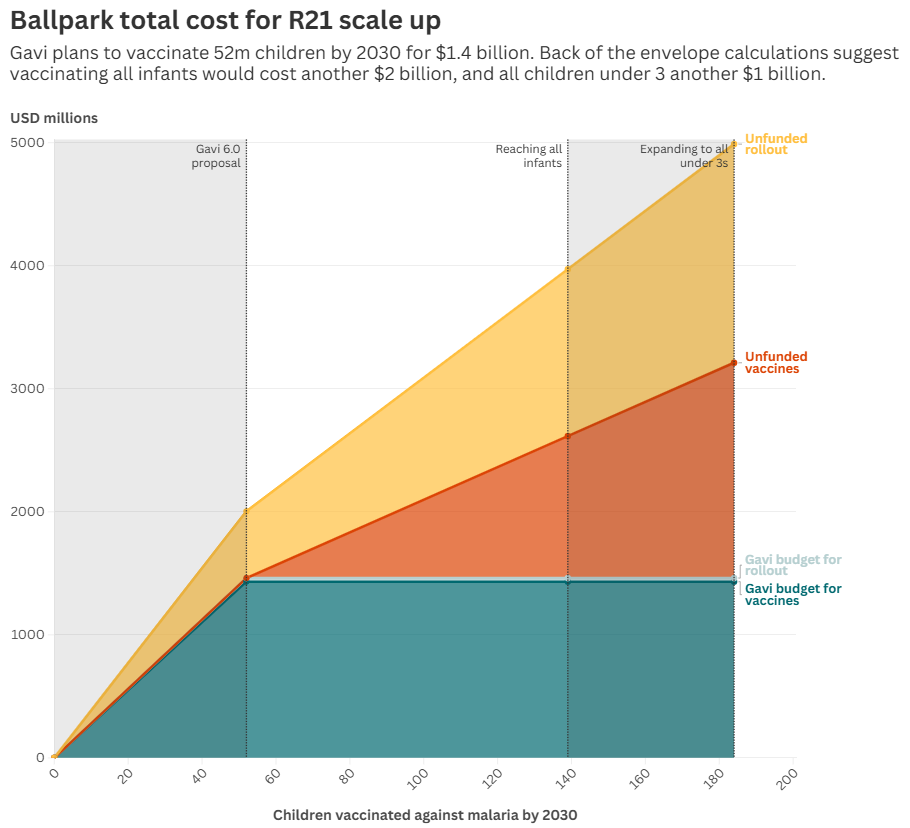
Sources: Authors’ calculations based on Gavi 6.0 business case, MVIP rollout costs, age-specific population of 20 countries with highest malaria incidence • Rollout costs are extremely conservative (i.e., high, reflecting full per child cost of the pilot, which is unlikely to be replicated at greater scale).
Zacharia Kafuko, Africa Director of 1Day Sooner, emphasized: “The lives of millions of children depend on swift action. The science is clear, and the infrastructure as well as the vaccine supply capacity exists. We lack sufficient funding from high-income countries, multilateral agencies, and philanthropists to bridge this gap and bring vaccines to those who need them most.”
The global fight against malaria stands at a critical juncture. Two new malaria vaccines, including R21, entered routine administration in 2024 and are projected to save 180,000 children’s lives by 2030. Yet, under current plans, an estimated 2.5 million children will die of malaria unvaccinated over the same period.
While Gavi, the Vaccine Alliance, has allocated $1.5 billion, this covers only one-third of the estimated $4–5 billion needed to vaccinate all eligible children by 2030. This funding gap is particularly pronounced in Nigeria, which accounts for a third of global malaria deaths and has a total health budget of just $10 per capita. Similarly, Angola, categorized as “fully self-financing” since 2018 (meaning that the country does not qualify to receive Gavi support for its vaccination campaigns), struggles to fund its vaccination programs due to recent economic setbacks. Unlike Nigeria, which receives Gavi support but faces a funding gap, Angola’s self-financing status means it must fully fund its vaccination programs, presenting a different challenge.
The White Paper also notes that poorer countries like the Democratic Republic of Congo, despite receiving highly subsidized vaccines, struggle with the “last-mile” issues of vaccine delivery and face significant logistical challenges, including community outreach and cold-chain management, to ensure uptake of the four-dose regimen.
The history of malaria is marked by excruciatingly long delays between the discovery of treatments and their widespread availability. From quinine’s scarcity in the 1600s to decades of regulatory hurdles for modern artemisinin therapies, progress has been slow. The same holds for malaria vaccines—research for the RTS,S vaccine began in the 1990s, with widespread use only starting in 2022.
Today, R21, a newer, more affordable vaccine with nearly unlimited production capacity, offers an unprecedented opportunity to turn the tide against malaria. However, despite its potential, challenges remain. According to the White Paper, “While supply constraints have eased, funding remains the primary obstacle.”
If fully funded, the rollout could transform health outcomes across 20 high-burden countries, including Benin, Burkina Faso, Mozambique, and the Democratic Republic of Congo. Yet, Gavi’s current allocation of $1.5 billion—intended to vaccinate 52 million children—covers only a fraction of the need.
Jean-Vincent Lamien, a 2023 Mandela Washington Fellow from Burkina Faso and a leading advocate for malaria eradication, stated: “This is a race against time. Every delay means preventable deaths. Collaboration across sectors and regions is the only way to ensure these vaccines’ equitable and timely rollout. The impact of such a collective effort would reverberate through generations.”
Logistical hurdles also hinder vaccine deployment. Ghana, Kenya, and Malawi, which piloted malaria vaccine programs, incurred additional costs of $2.75 per dose for community outreach and retention. Despite these efforts, only 39% of children completed the four-dose regimen, underscoring the need for comprehensive support beyond vaccine procurement.
Non-experimental results further highlight the importance of full vaccination. In Western Kenya, unvaccinated children were three times more likely to contract malaria than those with one dose of RTS,S, while partially vaccinated children remained six times more vulnerable compared to those completing the regimen.
The financial picture highlights an opportunity for impact at an unprecedented scale. Immediate investments of $500 million to strengthen rollout could mean the difference between lives saved and vaccines wasted. A further $2 billion could vaccinate 87 million additional infants in high-burden countries by 2030. Another $1 billion could reach 45 million older children who currently fall outside eligibility criteria, extending the vaccines’ life-saving benefits to those most in need.
While high-income countries, multilateral organizations, and philanthropists are urged to act decisively, the challenge extends beyond financial contributions. Effective vaccine deployment requires investments in community mobilization, cold-chain infrastructure, and healthcare workforce training to ensure every child in malaria-endemic regions is reached.
Distributed by African Media Agency (AMA) on behalf of 1Day Sooner.
About 1Day Sooner
1Day Sooner, a U.S.-based nonprofit, is dedicated to accelerating the development and deployment of life-saving medical research and policy interventions. 1Day Africa, as its African chapter, is committed to advancing the continent’s capabilities in local medical research and healthcare delivery, particularly for infectious diseases.
Read the full white paper here.
For more information, visit www.1daysooner.org or follow them on LinkedIn, X, and Bluesky.
For Media Inquiries Contact
Mbali Mpolokeng
Communications Consultant
Cell No. +27 65 921 8338
mbali@africacommunicationsgroup.com